Cataract
Bring the world into focus and get the vision you've always wanted. Talk to our doctors about your options today.
Premium Lens Cataract Surgery
As advancements in cataract technology continue, patients are able to get better vision without glasses in order to live the kind of lifestyle they want for themselves.
Light Adjustable Lens
The light adjustable lens is the first and only intraocular lens that can be adjusted after the surgery.
CATARACT SURGERY
see the world in a new light...
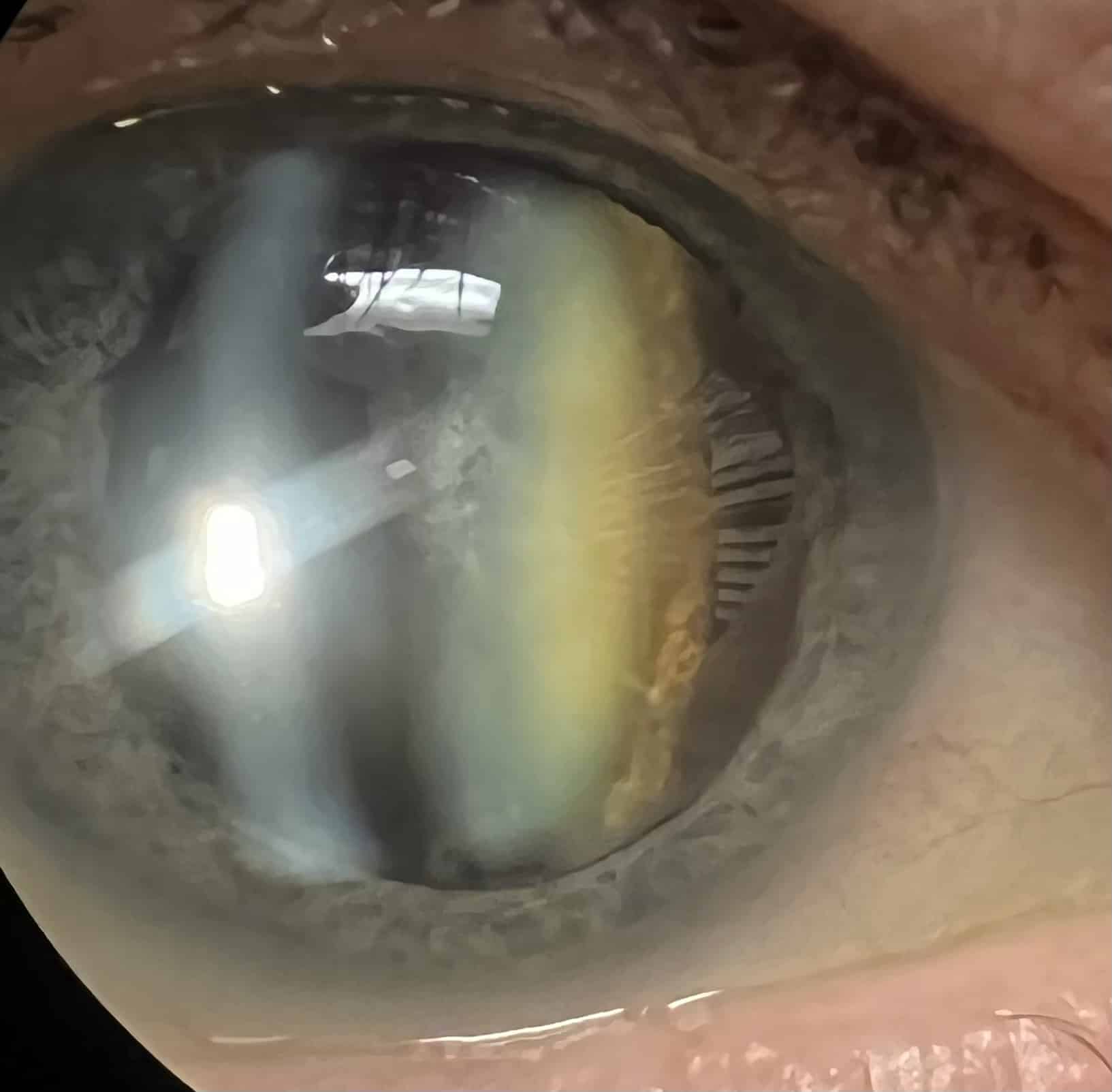
What is a Cataract?
A Cataract is a clouding of the natural lens inside the eye making it difficult for light to pass through.
At birth, we have a clear and flexible lens inside the eye that helps to focus images from near and far by changing its shape. The first age-related change we all experience is the loss of flexibility of the natural, clear lens. This generally occurs in our early 40’s and is the reason many begin to wear reading glasses or bifocals. As we age through our 40’s and 50’s, the degree of flexibility diminishes, which is why the amount of power needed for reading increases from a +1.00 to ultimately +2.00 to +2.50 reader. During this early change, the lens is generally clear. As we continue to age, the lens becomes cloudier, making it difficult to see clearly even with the aid of glasses. This is known as a cataract.
Cataracts are a natural part of the aging process and most people will develop them at some point in their lives. They can also be caused by other factors such as certain medical conditions (example: diabetes), medications (example: steroids) or eye injuries.
Common symptoms of Cataracts include





What is the Treatment for Cataracts?
The treatment for cataracts is surgery. Approximately 4 million cataract surgeries are performed every year.
During the procedure, a small incision is made in the cornea and the cataract is broken into small pieces to be removed, a process called phacoemulsification. After the old cataract is removed, it is replaced with a clear artificial lens called an intraocular lens or IOL. This helps restore clear vision and can dramatically improve the quality of life for those with cataracts. During the initial cataract consultation, many measurements of the eye are taken and the doctor will discuss the different intraocular lens options (more on this video)
Is it Laser Surgery?
Our surgeons are certified to perform femtosecond laser-assisted cataract surgery, have used, and have been certified on several laser platforms. However, multiple studies have shown no increase in accuracy or safety with the use of femtosecond laser in cataract surgery. Some of those studies have even suggested an increased risk of complications. The femtosecond laser is not covered by medical insurance, incurring a significant additional cost to the patient. As such, our surgeons do not recommend laser-assisted cataract surgery as it is an additional expense without a clear benefit.
When do I need Cataract Surgery?
Cataract surgery is generally indicated when one’s vision is poor enough to affect one’s activities of daily living despite the use of corrective glasses. The exact timing of surgery is variable as some feel they see and function well despite having cataracts. If a patient is overall happy with their vision, cataracts can be observed with yearly eye exams until they become symptomatic enough to require surgery.
Is Cataract Surgery covered by Insurance?
When cataracts become visually significant, the surgery would be covered by medical insurance companies (not vision plans). Some patients will have a deductible or co-pay; our staff can help determine that amount that would be due. There are options for premium lens placement during cataract surgery if there is a desire to reduce the need for glasses. Premium lens options would incur additional costs not covered by medical insurance. The surgery would still be covered but not the premium lens fees. These costs would be passed directly to the patient. Financing via alphaeon credit is available.
Where is surgery done and what is the recovery?
Cataract surgery is performed in an outpatient surgery center. Most can expect to be at the surgery center for approximately 3 hours going through the different steps at the facility (waiting time is built in!). Patients will get an IV placed so that the anesthesia team can deliver light sedation, which includes fast acting pain and anxiety medications. For any patients with high anxiety, the IV provides a fast way to deliver any additional medication needed. The eye is anesthetized topically with numbing medication.
While most are not fully asleep, the sedation can make patients forget they were in the operating room. On average, the procedure lasts 5-15 minutes. After surgery, there will be a post-operative check either that afternoon or the next day. Some patients will note an improvement to their vision the next day, while others may still be dilated and take a few days.
There will be eye drops to use for approximately 4 weeks after the procedure. There is typically minimal to no pain after the procedure. There are some restrictions after surgery (please review the instruction sheet given in post-op). Patients can drive 24 hours after the surgery if they are comfortable. Please note, patients still need someone to drive them to their postoperative visit. Surgery is done one eye at a time for safety reasons; the two eyes are often done 1-2 weeks apart.
Will cataracts come back?
No. Once cataracts are removed, they do not come back. Some patients will develop scar tissue behind the lens implant, known as posterior capsular opacification, that can blur the vision in a similar way cataracts can. If this occurs, it can be treated in the office with a laser, often leading to visual improvement by the next day. This procedure is called a capsulotomy. There are no special postoperative instructions after it is performed. The laser is covered by insurance. Like cataracts, this is a one-time treatment; the scar tissue does not recur once the laser is performed.
When can I update my glasses?
Glasses will need to be updated after cataract surgery. This is generally done 3-4 weeks after surgery to ensure stability.
Premium Lens Cataract Surgery
As advancements in cataract technology continue, patients are able to get better vision without glasses in order to live the kind of lifestyle they want for themselves. With so many lenses to choose from, it is important that your surgeon understands the goals of your lifestyle after cataract surgery. This is why all consultation regarding cataract surgery is done by the surgeon here at Eye Associates of Central Texas. We always want patients to understand that there is no “best lens,” just the right lens for you
We pride ourselves in offering the latest and best intraocular lenses. Currently, we are one of the only practices in the area offering the Light adjustable Lens. This is the only lens on the market that can be adjusted after the surgery is done!
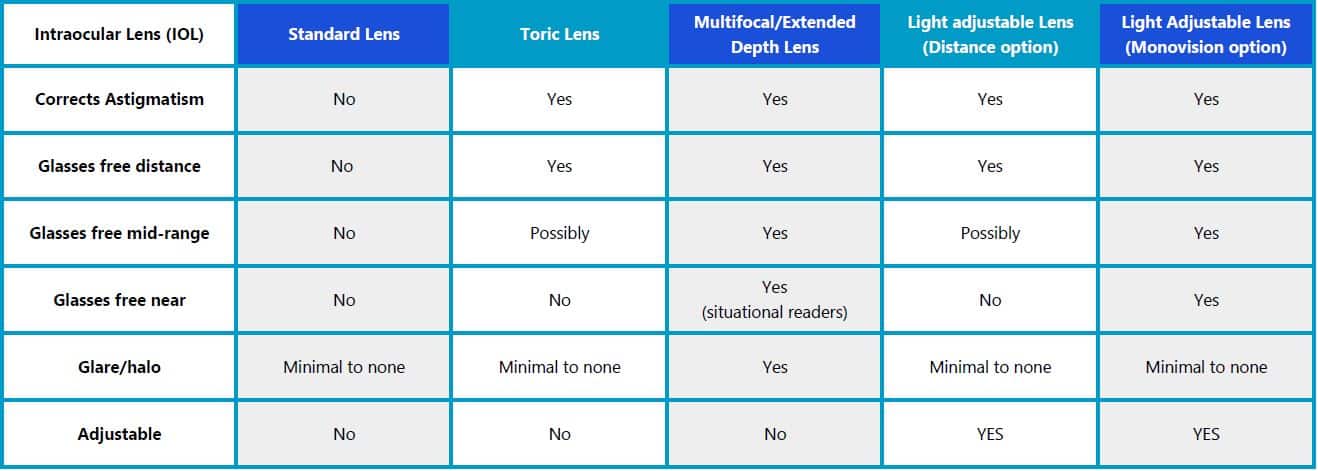
Standard Lens
The standard lens is the lens covered by medical insurance. This lens is a single-focus lens that can be set for distance, mid-range, or near vision. Because the lens is single-focus and cannot correct for astigmatism, it is expected that most patients will wear glasses in the form of a bifocal, trifocal, or progressive in order to focus at all ranges. There are some patients who have no or minimal astigmatism who may see well at the range that the lens is set to and only need glasses for the other two ranges. This lens is great for the patient who does not mind wearing glasses full-time after cataract surgery.
Toric lens
The Toric lens is an astigmatism correcting single-focus lens. This lens is designed to provide more clarity at the chosen focal point without glasses when compared to the standard lens for patients who have astigmatism. During the initial cataract consultation, several measurements of the eye are taken to measure both the amount and orientation of the astigmatism on the cornea. This information is then used to calculate the amount of astigmatism correction needed in the toric lens. During surgery, the lens is oriented in the eye to correct the astigmatism
As mentioned, the toric lens is a single-focus lens that makes one of the three focal points clear without glasses. Most choose the toric lens to be focused at distance; reading glasses would still be needed for mid-range and near activities.
Light Adjustable Lenses
Light Adjustable Lenses
The Light Adjustable Lens (LAL) is the world’s first lens implant that can be truly customized to your eye and visual requirements. With the LAL, you can test drive different vision settings. This customization allows you to have your personal ideal eyesight, reducing or even eliminating the need for eyeglasses in most daily situations.
What is the Light Adjustable Lens?
The Light Adjustable Lens (LAL) is the world’s first lens implant that can be truly customized to your eye and visual requirements. With the LAL, you can test drive different vision settings. This customization allows you to have your personal ideal eyesight, reducing or even eliminating the need for eyeglasses in most daily situations.
How does it work?
Once the LAL is in your eye and it has healed, your surgeon uses a Light Delivery Device (LDD) to finely-tune the power (prescription) of the lens. You may have up to three adjustments to find the best vision for you. Between adjustments, you can preview your eyesight and compare the different prescriptions. It may take a few treatments to perfect your results, but every adjustment gets you closer to your desired vision.
Who is a good candidate for the Light Adjustable Lens?
Most patients are ideal candidates to have the LAL, particularly if they want most precise vision possible and have a desire to eliminate the need for eyeglasses. You should not receive the LAL if you have:
- Significant pre-existing macular disease
- Sensitivity to UV light
- Uncontrollable eye movements
- History of herpes in the eye
You also need to be able to follow your eye doctor’s instructions closely. After receiving the LAL, you must wear special UV-protective glasses for approximately four to six weeks. If you are not prepared to follow these instructions, you should discuss other options with your doctor.
How many light treatments do I need?
The number of treatments depends on the shape of your eye, your prescription, and your personal preferences. You might need anywhere from two to four treatments total. Each light treatment is very brief, and they take place over one to two weeks. There is a good chance that you will achieve your desired vision within a month of having cataract surgery.
What makes the Light Adjustable Lens different from other IOLs?
During cataract surgery, your clouded lens gets replaced with an IOL. This method is successful at removing cataracts, but most patients still need glasses after surgery. There is no way to predict how your eye will heal, and other IOLs do not allow for adjustment after healing. The Light Adjustable Lens is different. It is the first and only adjustable IOL. That means you can customize your vision with the LAL based on your needs and desires after it has been implanted in your eye.
How can I find out if the Light Adjustable Lens is suitable for me?
You can learn more about the LAL and determine if it is right for you by talking to your eye doctor. If you are going to have cataract surgery, make sure to discuss your options before selecting an IOL. Your doctor will review your medical history and eye exams to determine if you’re a good candidate.
CORNEA & EXTERNAL DISEASE
let your light shine everyday
What is the Cornea?
The cornea is the clear window in front of your eye that focuses light and allows you to see.
Corneal Transplant Surgery
A normal cornea is naturally clear. If a patient has any scarring or disease on the cornea it can affect vision. In the past, the entire cornea had to be replaced during surgery, but now only a portion of the cornea can be removed. DSAEK and DMEK and DALK are types of partial cornea transplantation surgeries that increase recovery time and decrease potential complications of having a full thickness transplantation.
- Pentrating Keratoplasty (PKP) is a full thickness corneal transplant. This is performed when multiple layers of the cornea are cloudy or unhealthy.
- Descemet's Stripping Endothelial Keratoplasty (DSEK) is a partial thickness corneal transplant. This is performed when only a few layers of the cornea need to be replaced. Fuch's Dystrophy or Bullous Keratopathy are diseases that may require a partial corneal transplant.
- Descemet's Membrane Endothelial Keratoplasty (DMEK) is the newest type of partial thickness transplant. It only replaces 1 layer of the cornea and has the fastest recovery time.
- Deep Anterior Lamellar Keratoplasty (DALK) is a partial corneal transplant reserved for anterior corneal scarring or Keratoconus.
Dr. Lena Dixit and Dr. Ravi Patel of Eye Associates of Central Texas are Board-Certified and fellowship trained in Cornea and External disease. Both Dr. Dixit and Dr. Patel studied at Bascom Palmer Eye Institute, the top-ranked eye hospital in the nation. They specialize in the most current and advanced corneal procedures available. Dr. Dixit and Dr. Patel are amongst the few cornea, external disease, and refractive surgery specialists practicing in this area.

LASIK & PRK
transform vision into reality
LASIK & PRK
What is a Refractive Surgery?
Refractive surgery, such as LASIK and PRK, corrects nearsightedness, farsightedness and astigmatism, allowing you to be glasses-free. We are proud to offer Custom Wavefront-guided LASIK and PRK, state-of-the-art technology that creates a unique treatment based on a measurement that maps how your eye sees a single point of light – a treatment as unique as your fingerprint.
Eye Associates of Central Texas offers the highly advanced IntraLase Method. IntraLase is the same as LASIK; however, instead of a blade creating the flap in the cornea as with LASIK, a special laser creates the flap during IntraLase. IntraLase is commonly referred to as “blade-free” or “all-laser” LASIK. With IntraLase, LASIK is completely blade-free and safer than ever. The IntraLase FS laser is the first technology for a truly all-laser, blade-free LASIK procedure, replacing the hand-held microkeratome blade historically used in creating LASIK corneal flaps – the first step of the procedure – with a computer-guided, ultra-fast femtosecond laser. The IntraLase laser virtually eliminates the majority of the most severe sight-threatening LASIK complications related to use of the microkeratome and, by creating an optimal corneal surface below the flap, provides for better visual outcomes. IntraLase is the LASIK advancement you’ve been waiting for.
LASIK vs PRK
Laser-assisted in situ keratomileusis (LASIK) is a type of refractive surgery that utilizes a corneal flap. The healing process and visual recovery is quicker than PRK.
Photorefractive Keratectomy (PRK) is a type of refractive surgery that does not require a corneal flap, therefore has a slightly lower side effect profile. This is a great option for highly active individuals who wish to be glasses-free.
REFRACTIVE LENS EXCHANGE
Refractive lens exchange, or clear lens exchange, is an intraocular surgery that removes the natural lens in your eye and replaces it with a prescription artificial lens. This allows you to reduce the need for glasses or contact lenses in individuals that have high hyperopia or myopia. Ask your surgeon if you are a candidate today.
ROUTINE EYE EXAMS
illuminate the path of life
Routine Eye Exams
How do I know if I need an eye exam?
That is an answer that depends on many factors. The American Academy of Ophthalmology recommends that asymptomatic healthy patients should receive periodic eye examinations. Under the age of 40, it is recommended to have an exam every 5-10 years. From 40-54, every 2-4 years. From 55-64, every 1-3 years, and over the age of 65, every 1-2 years.
These recommendations change, based on symptoms, previous eye history, medical problems, and significant family history. For example, patients who wear glasses or contact lenses need yearly eye examinations to update their prescriptions. A patient with Diabetes should have a full, dilated eye examination at least once yearly to check for signs of diabetic retinopathy. This should start at the time of diagnosis. If there are risk factors for glaucoma, such as strong family history, it is recommended to have an exam every 1-2 years starting at the age of 40. If an ocular disease is found on your examination, follow-ups may need to be more frequent, and your doctor will advise you of the recommended time interval for re-examination.
What are we looking for?
During your exam, your doctor is examining your whole eye. Routine eye examinations check for glasses (refractive error), glaucoma, macular degeneration, cataract, and overall health of the eye. It is not uncommon for your ophthalmologist to find things on an eye examination that lead to the diagnosis of systemic diseases such as diabetes, high blood pressure, or even cancer. If your doctor has any concerns for your eye or overall health, he or she will discuss it with you at the time of the examination and create a medical plan for you. Your ophthalmologist works extremely closely with your other medical doctors to coordinate the best possible care for your body. It is important to realize that early stages of many eye disease produce no symptoms and that early diagnosis and intervention can lead to improved outcomes particularly when concerning cataracts, glaucoma, macular degeneration, and diabetic retinopathy.
How do I maintain healthy eyes?
We often get this question during routine eye examinations and health screenings. The most important thing you can do for your eyes is maintain good general health. Eye disease is more common among patients who smoke, have conditions like diabetes and high blood pressure, and who take certain medications such as steroids, medications for autoimmune conditions, and medications for certain infections. It is also extremely important to wear the proper eye protection. In general, polarized sunglasses are recommended while outdoors to protect the eyes from UV light. Damage from UV light can contribute to many different eye problems, including cataract, macular degeneration, pterygium, and ocular cancers. Eye protection is also required during high impact sports, such as racquetball, as well certain hobbies or professions, such as welding, grinding, and construction work.
Diabetic Retinopathy
Diabetes can affect the eyes in many ways. Patients with elevated blood sugars can have swelling of the lens inside the eye, causing fluctuating or blurred vision and changes in refraction. Patients with diabetes also have a higher incidence of both cataract and glaucoma. Prolonged elevation in blood sugar can cause damage to the small blood vessels of the eye, causing a condition called diabetic retinopathy. Early on, the blood vessels can become weak, causing bleeding and/or swelling that leads to non-proliferative diabetic retinopathy. In more advanced cases, new blood vessels can form, a condition called proliferative diabetic retinopathy. Active bleeding and/or swelling requires more treatment for your eye with lasers, injections, or surgery. Many early signs of diabetic retinopathy are asymptomatic, and, therefore, it is important to get yearly eye exams (at minimum) for screening.
Macular Degeneration
Age Related Macular Degeneration affects a particular part of the retina called the macula. The macula is responsible for the central part of your vision. There are two types of macular degeneration, dry and wet. The dry kind of macular degeneration is a common finding amongst older adults. Early changes include thinning of the macula and deposits, called drusen. Early stages of dry macular degeneration are often asymptomatic, while more severe changes can cause central vision loss. There is no definitive treatment for dry macular degeneration, but, depending on the stage of the disease, AREDS 2 vitamins may be recommended to slow the progression. Wet macular degeneration tends to have a more profound effect on a patient’s vision. New blood vessels form, which can bleed or leak eventually causing scar formation and central vision loss. This can often be treated with intraocular injections. As with many eye diseases, outcomes are improved with early detection. It is important to get regular eye examinations to check for macular degeneration. Patients who smoke or who have a strong family history are at higher risk. If you have been diagnosed, it is also important to monitor your vision regularly with amsler grid testing. Your doctor will also discuss supplementation with AREDS 2 vitamins.
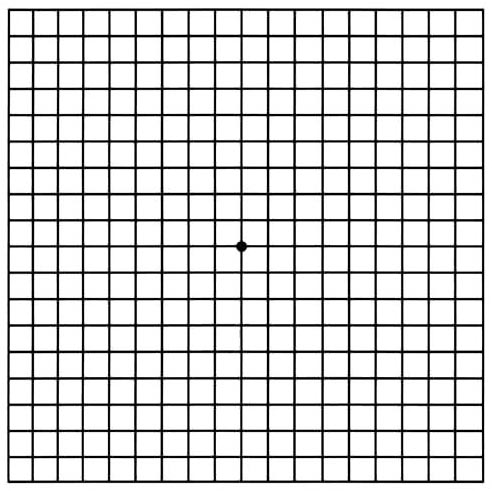
Amsler Grid for Macular Degeneration
Refraction
A refraction is the part of the exam that measures the optical focal point of your eye and provides the information needed to prescribe eyeglasses or contact lenses. You will have a phoropter device placed in front of your eyes (one at a time) and be asked to tell us which lens makes the vision more clear. Your ophthalmologist may also do a test called retinoscopy that is an objective way of determining your best possible vision. After testing a combination of lenses, we are able to write a prescription for glasses or contact lenses. The refraction also helps us to determine if you are a candidate for laser vision correction, or other types of refractive eye surgery.
Contact Lenses
Contact lenses require a specific exam to ensure good fit of the lens as well as good vision. Additionally, the health of your cornea must be assessed to see if you are a candidate for contact lenses. The refraction is used as a starting point to fit contact lenses. There are different types of contact lenses available, including 1 day, 2 week, and 4 week disposables as well as hard lenses. We will discuss which lens may be the best option for you. We will also spend time to educate you about proper lens use and replacement as well as good hygiene. It is important to remember never to sleep, shower, or swim in your contact lenses.
Dilation
Dilation is often part of the comprehensive eye examination. Patients are given eye drops that cause the pupil to enlarge. When the pupil is larger, the doctor is able to see to the back of the eye. This allows detailed examination of the lens, optic nerve, and retina. This is often necessary to ensure the good health of the eye. After dilation, patients may notice blurred vision, more noticeable for close ranges. The eyes will also be sensitive to bright lights. Therefore, it is important to wear sunglasses. The effects may last up to 4-6 hours.
Myopia
Myopia is also known as nearsightedness. This is a type of refractive error where objects up close appear clear but objects in the distance are blurry. This can be corrected with glasses, contacts, or refractive eye surgery
Hyperopia
Hyperopia is also known as farsightedness. This is a type of refractive error. Hyperopia is a bit of a misnomer because for a symptomatic patient, the vision is often not clear at any range. It may not be symptomatic until later in life. This can be corrected with glasses, contacts, or refractive eye surgery.
Presbyopia
Presbyopia is a type of refractive error that causes objects up close to be blurred. This is caused by age-related changes of the eye and usually becomes symptomatic after the age of 40. At first, one may find that holding the object farther away brings the object into focus. Using reading glasses can bring the object into focus without having to hold it farther away. Presbyopia can be corrected with glasses, contacts, or refractive eye surgery.
Our retina specialist, Dr. Oliver Fischer, offers medical and surgical treatment for:
- Diabetic Retinopathy
https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy - Age-Related Macular Degeneration (AMD)
https://www.aao.org/eye-health/diseases/amd-macular-degeneration - Epiretinal Membrane
https://eyewiki.aao.org/Epiretinal_Membrane - Retinal Vein Occlusion
https://www.aao.org/education/current-insight/retinal-vein-occlusion - Retinal Holes, Tears, Detachments
https://eyewiki.aao.org/Retinal_Detachment - Posterior Vitreous Detachment, flashes, floaters
https://www.aao.org/eye-health/diseases/what-is-posterior-vitreous-detachment - Macular Hole
https://www.aao.org/eye-health/diseases/what-is-macular-hole - Uveitis
https://www.aao.org/uveitis

Research
focus on innovation
Contact Us
Contact us at 512-244-1991 to see if you qualify for a research study.
Emergencies
If you have an emergency after regular business hours, you may contact your physician through TeleMed at 1-888-596-7908. In cases where emergency care is needed immediately, please go to the hospital emergency room nearest you.
Call our office today to speak with one of our staff who can give you an appointment.